Healthcare providers, meet Gravie.
Gravie is a licensed, third-party administrator that offers self-funded health plans for employers. We are here to make accessing care better for everyone — including our members’ healthcare providers.
Get ready for Gravie —
and get claims paid faster.
If you have additional questions, check out our Provider FAQs or give us a call at 877.684.3984.
STEP 1
For faster eligibility and benefits verification, add Gravie to your patient billing system today.
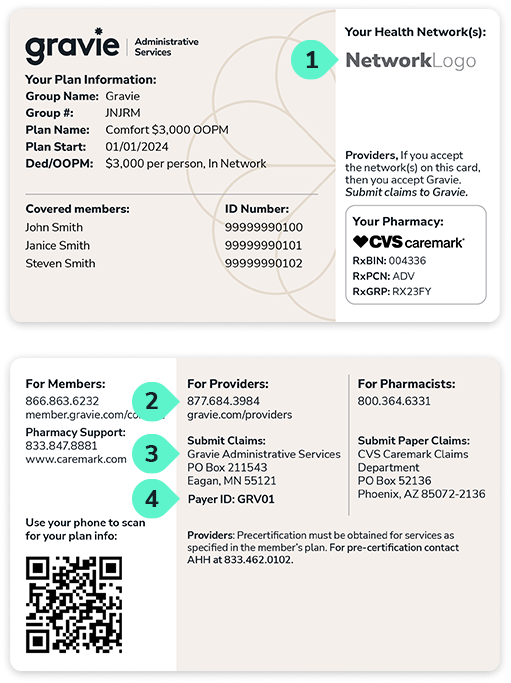
Be sure to enter Gravie’s information into the system your office uses to verify eligibility and submit claims. Some systems do not have a separate field for the plan administrator and the network, so many providers add something like “Gravie – Aetna” or “Gravie – Cigna” to their system’s drop-down menus.
Add a similar option to your website if you require patients to enter insurance information ahead of their visit.
STEP 2
Make sure your clearinghouse has
listed our Payer IDs.
If Gravie isn’t listed, please request that your clearinghouse update their payer ID list.
- Cards with an Aetna logo – Payer ID: GRV01
- Cards with a Cigna logo – Payer ID: 62308
Precertification Lists
Choose from the following links for instructions on how to request precertification for patients enrolled in Gravie health plans.
STEP 3
Register for our
provider portal.
In order to register as a new provider in the portal, you must have at least one paid claim already on file.
If you have not yet filed a claim, or if your claim is still pending, please call Gravie at 877.684.3984 to verify information on your patient’s eligibility and/or claim.
Once your patient has submitted a claim, download the instructions on how to register.
Submitting claims
Chances are, you already accept Gravie. If you see a network logo that you accept on our ID card, then you accept Gravie.
Benefits are administered through Gravie with primary and regional leased networks through
Aetna, Cigna, and PHCS/Multiplan.
If you don’t see our payer ID listed with your clearinghouse, please request that they update their payer ID list.
You can validate our payer ID by visiting the Smart Data Stream portal and searching for GRAVIE.

If your patient has an Aetna logo on their ID card and a 5-digit Group # (eg. EHDLK), submit claims electronically through the Smart Data Stream Portal, or mail to:
Payer ID: GRV01
Gravie Administrative Services
PO Box 211543
Eagan, MN 55121
If your patient has an Aetna logo on their ID card and an 8-digit Group # (eg. GRV12345), submit claims to:
Payer ID: 41147
Mail to:
Gravie Administrative Services
PO BOX 59212
Minneapolis MN 55459
For prior authorization and medical necessity, contact American Health Holdings:
Fax: 866.881.9643
Phone: 833.462.0102
For case management:
Fax: 866.353.6508
Phone: 800.641.3224

If your patient has a Cigna logo on their ID card, submit claims to:
Payer ID: 62308
Mail to:
Cigna
PO Box 188061
Chattanooga, TN 37422-8061
Prior authorization, case management, utilization management:
Contact Gravie at the provider services number on the back of the card.

If your patient has only a PHCS logo on their ID card, please submit claims to:
Payer ID: 36326
Mail to:
HealthEOS by Multiplan
PO Box 6090
De Pere, WI 54115-6090
Provider FAQs
As a healthcare provider, we know that your primary focus is on delivering great care to patients. To support you, we’ve gathered answers to some of the most common questions we receive in order to make your job as clear and straightforward as possible.
If your question isn’t answered here, please call our provider support team at 877.684.3984.
Patient Eligibility
You can find details on your patient’s benefits eligibility by accessing the Gravie Provider Portal. Simply log in and search for your patient’s group ID number. If you do not already have an account, please register here.
Follow these steps to troubleshoot any issues locating your patient in the portal:
- First, make sure you are searching for the member under Gravie Administrative Services in the Gravie provider portal, and not under Aetna/Cigna. Gravie leases the networks of Aetna and Cigna to access their providers, so the member will not show up under Aetna/Cigna. Please refer to the SUBMITTING CLAIMS section above for where to submit claims based on your patient’s ID card.
- Second, make sure you are searching for the member using either the Gravie Provider Portal.
- If your patient group ID number consists of 5 characters (e.g., AHTYJ), use the Gravie provider portal.
Still having issues? Contact Gravie Care at 877.684.3984.
Provider Portal Questions
Visit the Reset Password page on the portal to reset your login information. You will be able to use your email address to reset your account.
To update your preferred email address, log in to the Gravie Provider Portal, click Preferences in the upper-right corner of the portal, and update the email address on your profile.
Claims Status
To check the status of a claim, log in to the Gravie Provider Portal. Then navigate to the Claims tab and enter the requested information to pull up the claim in the system.
In general, claims take approximately 30 business days from the date of submission to when the payment is processed, though this may vary depending on the details of the claim. Please check the provider portal first for an updated status of your claim.
This could be for a few reasons. Follow these steps to determine why your claim may have not yet been processed:
- Incorrect Payer ID: It is possible that you are using an outdated Payer ID. Please make sure you are using either GRV01 (Aetna), 62308 (Cigna), or 36326 (MultiPlan) as the Payer ID.
- Claim sent to wrong address: Please verify that you’ve submitted your claim to the correct address based on your patient’s ID card, detailed in the SUBMITTING CLAIMS section above.
- Wrong member info: Please also verify the member’s ID information, as it is possible you are referencing the wrong ID card.
- 30 days to process: Please keep in mind that claims take approximately 30 days to process. If it’s been fewer than 30 days since you submitted a claim, please recheck the status at a later date.